
08 Dec Speed Up Tooth Extraction Recovery
Embarking on the road to recovery after a tooth extraction can conjure up a mix of relief and anxiety: relief that a source of pain or infection is gone, but anxiety about the healing process. Understanding what the days and weeks post-extraction should entail is crucial for a smooth and quick recovery. Whether you’ve had a wisdom tooth removed or a decayed tooth extracted, knowing how to care for your mouth, manage discomfort, and nourish your body during this delicate time is the cornerstone of a positive outcome. This essay aims to shed light on the effective strategies and essential steps that lay the foundation for a swift and successful healing journey after tooth extraction.
Post-Extraction Care
Post-Operative Oral Care: Essential Steps Following Tooth Extraction
A meticulous approach to oral care post-tooth extraction is paramount to facilitate optimal healing and prevent complications such as infection or alveolar osteitis, commonly referred to as dry socket. As researchers and practitioners in the field of dental medicine, a profound understanding of post-extraction care is critical. The following directive offers an evidence-based, thorough regime to ensure a patient’s prompt and uneventful recovery following tooth extraction.
Immediate Post-Extraction Care (First 24 hours):
- Hemostasis Maintenance: Upon completion of the extraction, a gauze pad will be placed over the surgical site. One must apply constant pressure by biting down gently for approximately 30-45 minutes. This pressure aids in the formation of a stable blood clot, an essential component of the healing process.
- Analgesic Administration: Pain management should begin promptly with the administration of prescribed analgesics or over-the-counter pain relief medications, such as acetaminophen or ibuprofen, as directed.
- Activity Moderation: Engaging in strenuous activity can provoke increased bleeding and should be avoided for 24 hours following extraction. Elevate the head with additional pillows during rest to minimize swelling.
Oral Care Protocol Post Extraction:
- Clot Preservation: The integrity of the blood clot within the socket is central to healing. One must abstain from smoking, using straws, or performing any suction movements with the mouth for at least 72 hours post-extraction.
- Oral Hygiene Adaptation: While regular oral hygiene should continue, it is advised to bypass the extraction site during tooth brushing and flossing for the first day. After 24 hours, one may gently rinse with warm saline solution (half a teaspoon of salt in a cup of warm water) to maintain cleanliness and reduce the risk of infection.
- Dietary Modifications: Immediately following extraction, a diet consisting of soft foods and ample liquids is recommended. Avoid hot liquids and foods, as they may dissolve the forming blood clot. As the extraction site begins to heal, one can gradually reintroduce more solid foods.
- Swelling Management: To mitigate swelling, apply an ice pack externally at the site of extraction in intervals of 10 minutes on and 20 minutes off.
- Medication Compliance: If an antibiotic was prescribed, it is crucial to complete the full course as directed to thwart potential infection.
- Avoidance of Irritants: One should shun alcohol consumption and mouthwashes containing alcohol for at least 24 hours as they can impede the healing process.
Follow-Up Practices:
- Alertness to Complications: Should there be signs of persistent or worsening pain, excessive bleeding, or fever, immediately contact a dental professional.
- Post-Operative Visitation: Attend scheduled follow-up appointments with the oral surgeon or dentist to ensure proper healing and to address any complications promptly.
Adherence to these essential post-operative care steps assures not only a reduction in discomfort but also primes the affected oral region for successful healing and restoration. It is with a dedication to dental health and knowledge of the underlying biological processes that these careful guidelines are prescribed for individuals recovering from tooth extraction.

Diet and Nutrition
Optimal Nutritional Intake for Expedited Recovery Post Tooth Extraction
Following the intricacies of hemostasis maintenance and the scrupulous modification of oral hygiene practices, patients’ dietary choices emerge as a pivotal factor in the convalescent phase post tooth extraction. A deliberate selection of alimentary substances can significantly impact the swiftness and efficacy of the recovery process.
Upon completion of an extraction procedure, the alimentary regimen ought to be tailored to avoid any undue stress upon the surgical site, whilst ensuring that all nutritional needs are met. In the initial stages, soft foods that require minimal masticatory effort are highly recommended. These include, but are not limited to, yogurt, applesauce, and lukewarm soups. Consumption of these items assists in preserving the integrity of the blood clot at the extraction site, a salient factor in the prevention of the deleterious condition known as dry socket.
Foods that are rich in vitamins and minerals, particularly those that promote wound healing such as vitamin C and zinc, should be actively sought. Citrus fruits, whilst rich in vitamin C, should be approached with caution due to their acidity. Alternative sources like sweet potatoes and leafy greens are more conducive to a conducive oral environment for healing. Protein is a crucial component for tissue repair; hence, a focus on easily consumable sources like scrambled eggs and cottage cheese is imperative.
In contrast, there are victuals that must be assiduously avoided to facilitate an auspicious recovery trajectory. Any food items that are of a hard, crunchy, or sticky consistency can disrupt the clot formation and exacerbate the wound. This includes nuts, chips, and candies, amongst others. Additionally, the intake of extremely hot or spicy foods can induce an inflammatory response, which is counterproductive to the healing process.
Patients are advised to abstain from the usage of straws, as the suction motion can pose a risk to the stability of the blood clot. Similarly, alcoholic beverages and those containing caffeine are to be avoided, as they can impair the body’s healing mechanisms through dehydration and increased risk of bleeding.
In conclusion, the consumption of a balanced diet that emphasizes soft, nutrient-dense foods, while meticulously avoiding those that may hinder the recovery process, is a cornerstone of a swift and successful recuperation post tooth extraction. It is this measured approach to nutrition that will ensure the body is duly equipped to repair and rebuild the affected oral tissues, minimizing discomfort and ensuring a return to optimal oral health in the shortest time possible.

Recognizing Complications
Assessment of Wound Healing after Dental Extractions: The Phenomenology of Recovery Processes and Indicators of Progress
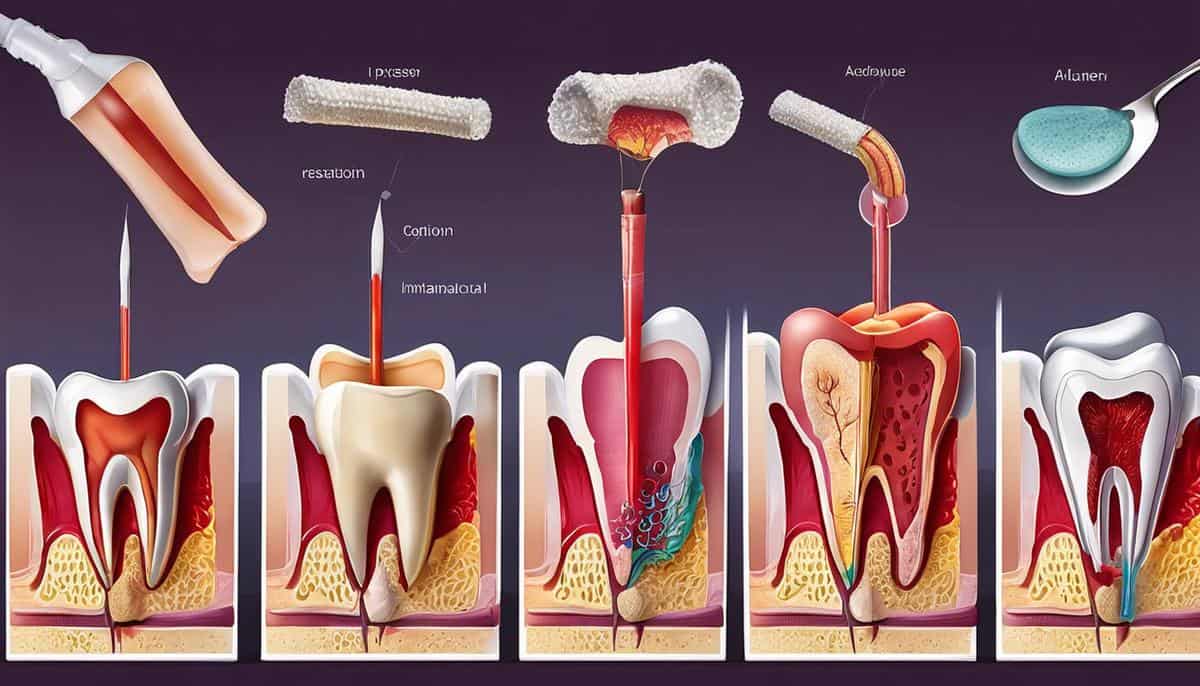
The healing trajectory of a tooth extraction site is a manifestation of the intricate interplay among cellular activities, tissue adaptation, and systemic factors. This complex progression of wound healing naturally transitions through phases of inflammation, proliferation, and maturation. However, recognizing the concrete signs of normal versus aberrant healing is paramount to ensure prompt interventions, should complications arise.
Normal healing processes are typically characterized by gradual diminishment of initial symptoms. As the extraction site heals, one should observe a sequential lessening of inflammation and pain. Tissue restoration commences with the formation of a well-established clot which then gets replaced by granulation tissue, an intermediary substrate that is rich in collagen and the foundation for new blood vessels. This substrate will eventually be supplanted by regenerated tissue integrated into the surrounding gingiva.
Objective indicators of proper healing include the absence of excessive inflammation beyond the initial post-operative period, coupled with pain that progressively subsides without escalating or persisting unexpectedly. Erythema, the reddish tinge commonly associated with inflammation, should reduce gradually within the first few days. Moreover, a consistent reduction in the size of the extraction socket indicates the space is being filled by the nascent granulation tissue.
Patient-reported outcomes, such as a decrement in discomfort and the ability to perform normal oral functions without pain, are essential subjective measures. Additionally, the timeline for healing should be accounted for; most extraction sites require a convalescence period of one to two weeks for primary soft tissue healing. A noticeable improvement in symptoms should be evident within this period.
Conversely, there are salient signs that might alert one to suboptimal healing trajectories, which necessitate professional examination. Infections, for instance, would present with worsening swelling, exacerbated pain, and possibly the presence of pus or an offensive odor emanating from the extraction site. Furthermore, the sensation of an unpleasant taste in the mouth often accompanies an infected extraction site. In the event of a dry socket, a condition where the blood clot is dislodged prematurely, one would experience severe pain, typically radiating to the ear, and a noticeable absence of a clot in the socket appearing as a dry-looking opening.
Persistent bleeding beyond the initial post-extraction period is also a sign that merits attention. While some oozing is common in the first few hours, continuous or recurrent bleeding may suggest inadequate clot formation or underlying systemic causes such as coagulopathy, and hence, requires dental assessment.
It is also crucial to observe the coloration and texture of the tissues surrounding the extraction site. Discolorations that progress to a darker shade, resembling bruising, are customary; however, persistence of such hues beyond the typical resolution time may indicate deeper tissue trauma or hemorrhage.
In sum, surveillance of the healing process after a dental extraction focuses on both objective cues and subjective experiences. This encompasses observing the reduction of inflammatory symptoms, the formation, and persistence of a proper clot, progressive tissue filling within the socket, and decreases in discomfort and functional impairment. Vigilance for symptoms that deviate from the expected healing curve, such as persistent pain, prolonged bleeding, or signs of infection, must prompt the seeking of dental expertise. Early detection and intervention are vital in addressing complications and ensuring a resumption of the healing process, ultimately leading to full tissue restitution.
As we navigate the path that leads from tooth extraction towards restored oral health, the role of informed self-care cannot be overstated. Adhering to a regimen of post-extraction care, embracing a diet conducive to healing, and remaining vigilant for any signs of complication are the linchpins of a smooth transition to recovery. Properly equipped with this knowledge, you can approach the healing process with a sense of control and confidence. Trust that with careful attention and a commitment to following professional guidance, you can emerge from the experience with a strong, healthy smile that stands the tests of time and tribulation.


Sorry, the comment form is closed at this time.